Pengaruh Pengunaan Alat Kontrasepsi dengan Kejadian Kematian Neonatal Dini
Effects of Contraceptive Use with the Incidence of Premature Neonatal Death
Keywords:
Family Planning, Mortality, Early NeonatalAbstract
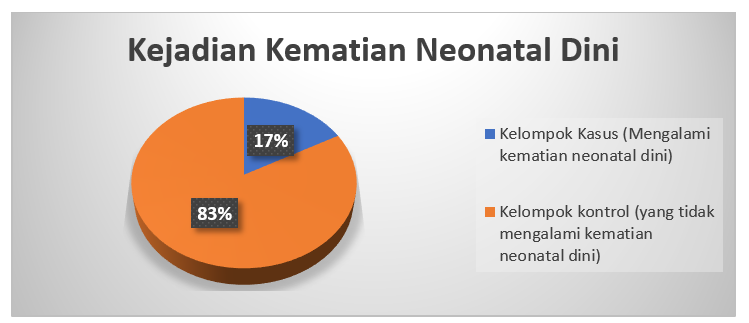
Introduction: Early Neonatal Death gave of 2/3 infact death. The purpose this study aim to the effect of family planning with early neonatal death. Methode: This study is a quantitative study with the design of case kontrol research at primary health care in Sarmi on June 1st - November 31st, 2020 with case samples are mothers who experienced early neonatal death of 34 people and kontrol samples are mothers who did not experience early neonatal events of 166 people with a ratio of 1: 5. This study uses medical record data in 2017-2019 Puskesmas Sarmi with logistic regression analysis of risk faktor models processed using STATA 14. Results: The results of this study indicate that there is an effect of using contraceptives on early neonatal mortality after being controlled by confounding variables such as gestational age, gestational age, LILA, Hb levels, and ethnicity (p value 0.0001 with an OR value of 11.4 (95%CI= 4.5 – 29.5). Optimization of care mentoring roles in efforts to increase PUS and WUS participation in the Birth Kontrol Program to prevent and reduce early neonatal deaths.
ABSTRAK
Pendahuluan: Kematian neonatal dini menyumbangkan sekitar 2/3 kematian anak. Tujuan: untuk melihat pengaruh penggunaan alat kontrasepsi dengan kematian neonatal dini. Metode: Penelitian ini merupakan penelitian kuantitatif dengan desain penelitian case kontrol yang dilakukan di Puskesmas Sarmi pada tanggal 1 Juni – 31 November 2020 dengan sampel kasus adalah ibu yang mengalami kejadian neonatal dini sejumlah 34 orang dan sampel kontrol adalah ibu yang tidak mengalami kejadian neonatal dini sejumlah 166 orang dengan perbandingan 1: 5. Penelitian ini menggunakan data rekam medik tahun 2017-2019 Puskesmas Sarmi dengan analisis logistic regression model faktor risiko yang diolah menggunakan STATA 14. Hasil: Hasil penelitian ini menunjukkan adanya pengaruh penggunaan alat kontrasepsi terhadap kematian neonatal dini setelah di kontrol oleh variabel konfoding berupa usia kehamilan, jarak kehamilan, LILA, Kadar Hb, dan suku (p value 0,0001 dengan nilai OR sebesar 11,4 (95% CI= 4,5 – 29,5). Optimalisasi peran pendampingan kader dalam upaya meningkatkan partisipasi PUS dan WUS pada Program KB untuk mencegah dan mengurangi kematian neonatal dini.
Downloads
References
Abdullah, A. Z., Naiem, M. F., & Mahmud, N. U. (2012). Faktor Risiko Kematian Neonatal Dini di Rumah Sakit Bersalin. Kesmas: National Public Health Journal, 6(6), 283. https://doi.org/10.21109/kesmas.v6i6.83
Balitbang Kemkes. (2020). Studi Status Gizi Balita Teringrasi Susenas 2019. In Balitbangkes Kemenkes RI (Issue 2020). https://persi.or.id/wp-content/uploads/2020/11/event8-02.pdf
Bangun, I. F., Abdiana, A., & Edison, E. (2019). Faktor Risiko Kematian Neonatal di Kabupaten Kepulauan Mentawai. Jurnal Endurance, 4(1), 26. https://doi.org/10.22216/jen.v4i1.3641
Biore, T. (2018). Hubungan Determinan Sosial Kesehatan terhadap Kematian Neonatal [Trisakti]. http://repository.trisakti.ac.id/usaktiana/index.php/home/detail/detail_koleksi/0/SKR/judul/00000000000000096455/#
Cleland, J., Bernstein, S., Ezeh, A., Faundes, A., Glasier, A., & Innis, J. (2016). Family planning: the unfinished agenda. Lancet, 368(9549), 1810–1827. https://doi.org/10.1016/S0140-6736(06)69480-4
Dahiru, T. (2016). Determinants of Early Neonatal Mortality in Nigeria: Results from 2013 Nigeria DHS. Journal of Pediatrics & Neonatal Care, 2(5), 1–8. https://doi.org/10.15406/jpnc.2015.02.00089
Dinas Kesehatan Provinsi Papua. (2021). Profil Kesehatan Provinsi Papua Tahun 2021. https://dinkes.papua.go.id/informasi-publik/informasi-berkala/
Elder, T. E., Goddeeris, J. H., & Haider, S. J. (2016). Racial and Ethnic Infant Mortality Gaps and The Role of Socio Economic Status. Pubmed Central, 176(1), 139–148. https://doi.org/10.1016/j.labeco.2016.04.001.Racial
European Union, INFID, Koalisi Perempuan Indonesia, & OXFAM. (2020). Tujuan 03 (Kesehatan yang Baik dan Kesejahteraan). SDGs Indonesia. https://www.sdg2030indonesia.org/page/11-tujuan-tiga
Katadata. (2020). Kematian Balita di Indonesia Capai 28,2 Ribu pada 2020. Datanoks. https://databoks.katadata.co.id/datapublish/2021/10/22/kematian-balita-di-indonesia-capai-282-ribu-pada-2020#:~:text=Kematian%20bayi%20berusia%20di%20bawah,bulan%20(post%2Dneonatal).
Kemenkes RI. (2021). Profil Kesehatan Indonesia 2020. In Kementrian Kesehatan Republik Indonesia. Kementerian Kesehatan Republik Indonesia. https://pusdatin.kemkes.go.id/resources/download/pusdatin/profil-kesehatan-indonesia/Profil-Kesehatan-Indonesia-Tahun-2020.pdf
Kibria, G. M. Al, Burrowes, V., Choudhury, A., Sharmeen, A., Ghosh, S., Mahmud, A., & Angela, K. C. (2018). Determinants of Early Neonatal Mortality in Afghanistan: An Analysis of the Demographic and Health Survey 2015. Globalization and Health, 14(1), 1–12. https://doi.org/10.1186/s12992-018-0363-8
Lwanga, S. K., & Lemeshow, S. (1991). Sampel Size Determination in Health Studies. WHO. https://apps.who.int/iris/bitstream/handle/10665/40062/9241544058_%28p1-p22%29.pdf?sequence=1&isAllowed=y
Matahari, R., Utami, F. P., & Sugiharti, S. (2018). Buku Ajar Keluarga Berencana Dan Kontrasepsi. In R. Sofianingsih (Ed.), Pustaka Ilmu. http://eprints.uad.ac.id/24374/1/buku ajar Keluarga Berencana dan Kontrasepsi.pdf
Mosley, W.H & Chen, L. . (1984). An Analytical Framework for the Study of Child Survival in Developing Countries. Population and Development Review, 25(45), 140–145. https://www.jstor.org/stable/2807954
Noviani, A., Sari, M., Septina, H. R., & Hardianto. (2020). Profil Kesehatan Ibu Dan Anak 2020. In Badan Pusat Statistik (pp. 126-). BPS. https://www.bps.go.id/publication/2020/12/31/b9a9aa33ab5a3cc23311d0a1/profil-kesehatan-ibu-dan-anak-2020.html
Nugraheni, A., Mahkota, R., & Adisasmita, A. C. (2016). Pengaruh Komplikasi Kehamilan terhadap Kematian Neonatal Dini Indonesia (Analisis Data SDKI 2007). Media Medika Muda, 1(1), 57–66. https://ejournal2.undip.ac.id/index.php/mmm/article/view/2572
Oktarina, S., Fajar, N. A., & Yeni. (2017). Model Prediksi Kejadian Kematian Neonatal Di Kecamatan Purbolinggo Kabupaten Lampung Timur Provinsi Lampung. Jurnal Ilmu Kesehatan Masyarakat, 8(1), 49–55. https://repository.unsri.ac.id/28991/1/JIKM Prediksi Kematian Neonatal.pdf
PKM Sarmi. (2020). Laporan Kasus Kematian Ibu dan Anak Puskesmas Sarmi Tahun 2020.
Prawirohardjo, S. (2019). Ilmu Bedah Kebidanan. In S. P. & H. Winkjosastro (Ed.), Yayasan Pustaka Sarwono Prawirohardjo (7th ed., Vol. 7). Yayasan Pustaka Sarwono Prawirohardjo.
Prawiroharjo, S. (2018). Ilmu Kebidanan. In A. B. Saifuddin (Ed.), Edisi keenam. PT. Bina Pustaka Sarwono Prawirohardjo.
Putri, A. R., & Al Muqsith. (2016). Hubungan Lingkar Lengan Atas Ibu Hamil dengan Berat Badan Lahir Bayi di Rumah Sakit Umum Cut Meutia Kabupaten Aceh Utara dan Rumah Sakit Tk IV IM.07.01 Lhokseumawe Tahun 2015. Averrous Jurnal Kedokteran Dan Kesehatan Malikussaleh, 2(1), 1–8. https://repository.unimal.ac.id/3053/1/Jurnal averrous (LILA).pdf
Rachmadian, A. P., Shodikin, M. A., & Komariah, C. (2018). Faktor-Faktor Risiko Kematian Bayi Usia 0-28 Hari di RSD dr. Soebandi Kabupaten Jember. Journal of Agromedicine and Medical Sciences, 4(2), 59–65. https://repository.unej.ac.id/handle/123456789/86309
Raharni, R., Isakh, B., & Diana, I. (2012). Profil Kematian Neonatal Berdasarkan Sosio Demografi Dan Kondisi Ibu Saat Hamil Di Indonesia. Buletin Penelitian Sistem Kesehatan, 14(4 Okt), 391–398. https://doi.org/10.22435/bpsk.v14i4
Ravelli, A. C. J., Tromp, M., Huis, M. M. Van, Steegers, E. P., Tamminga, P., Eskes, M., Bonsel, G. J., Ravelli, A. C. J., Tromp, M., Huis, M. M. Van, Steegers, E. P., & Tamminga, P. (2017). Decreasing Perinatal Mortality in The Netherlands , 2000-2006 : a Record Linkage Study. 2000–2006. https://hal.archives-ouvertes.fr/hal-00477871
Sari, I. P., Ardillah, Y., & Widyastuti, T. A. (2016). The Determinants of Infant Mortality in Neonatal Period. Jurnal Kesehatan Masyarakat, 12(1), 139–149. https://doi.org/10.15294/kemas.v12i1.4882
Sari, R. D., Sutyarso, Bakri, S., Dyah Wulan Sumekar, R. W., Suryawinata, A., Mentari Olivia, F., & Mahdiansari, T. (2020). Maternal Health Study in Province Lampung Based on Prediction Model Structural Equation Modeling-Partial Least Square. European Journal of Contraception and Reproductive Health Care J Mol Clin Med, 7(3), 4727–4735. https://www.embase.com/search/results?subaction=viewrecord&id=L2010488918&from=export
Sekardira, R. A., Sulistiawati, & Etika, R. (2020). Faktor Risiko Kematian Neonatal. UNAIR News, 7–8. http://news.unair.ac.id/2020/12/22/faktor-risiko-kematian-neonatal/
Shah, R. (2018). Action on the Call Ending Preventable Child and Maternal Deaths. In USAID. USAID. https://doi.org/10.1044/leader.ppl.19062014.20
Singh, S., Darroch, J., Ashford, L., & Vlassof, M. (2018). Adding It Up: The Costs and Benefits of Investing in Family Planning and Maternal and Newborn Health. In New York: Guttmacher Institute and United Nations Population Fund (UNFPA). https://www.guttmacher.org/sites/default/files/report_pdf/AddingItUp2009.pdf
Susanty, S. D., Agus, S., & Santy, R. (2016). Kajian Faktor-Faktor Penyebab Kematian Bayi di Kota Padang. Maternal Child and Health Care, 3(6). https://ojs.fdk.ac.id/index.php/humancare/article/view/80
UN. (2016). Levels and Trends of Contraceptive Use as Assessed In 2002 (Issue ST/ESA/SER.A/239). Department of Economic and Social Affairs Population Division ST/ESA/SER.A/239 LEVELS. http://www.un.org/esa/population/publications/publications.htm
WHO. (2016, November). Perinatal and Neonatal Mortality Country, Regional dan Global Estimates. WHO. https://doi.org/10.1136/bmj.281.6254.1567-b
WHO. (2020a). Newborns: improving survival and well-being. World Health Organisation, Mlcc, 1–5. https://www.who.int/news-room/fact-sheets/detail/newborns-reducing-mortality
WHO. (2020b). World Health Statistic 2020 (Monitoring Health For SDGs) (Issue 1). WHO. https://apps.who.int/iris/bitstream/handle/10665/332070/9789240005105-eng.pdf
WHO. (2021). World Health Statistic 2021 (Monitoring Health For The SDGs). https://apps.who.int/iris/bitstream/handle/10665/342703/9789240027053-eng.pdf
WHO, & UNICEF. (2017). Reaching the Every Newborn National 2020 Milestones Country Progress, Plans and Moving Forward (Issue May). WHO & UNICEF. http://apps.who.int/iris/bitstream/10665/255719/1/9789241512619-eng.pdf?ua=1
Xinxo, S., Bimbashi, A., Kakarriqi, E., & Zaimi, E. (2017). Association Between Maternal Nutritional Status of Pre Pregnancy, Gestational Weight Gain and Preterm Birth. Materia Socio Medica, 25(1), 6. https://doi.org/10.5455/msm.2013.25.6-8
Published
How to Cite
Issue
Section
Copyright (c) 2022 Authors

This work is licensed under a Creative Commons Attribution-ShareAlike 4.0 International License.
Authors who publish with Jurnal Bidan Cerdas agree to the following terms:
- Authors retain copyright and grant the journal right of first publication with the work simultaneously licensed under a Creative Commons Attribution License (CC BY-SA 4.0) that allows others to share the work with an acknowledgment of the work's authorship and initial publication in this journal.
- Authors are able to enter into separate, additional contractual arrangements for the non-exclusive distribution of the journal's published version of the work (e.g., post it to an institutional repository or publish it in a book), with an acknowledgment of its initial publication in this journal.
- Authors are permitted and encouraged to post their work online (e.g., in institutional repositories or on their website) prior to and during the submission process, as it can lead to productive exchanges, as well as earlier and greater citation of published work.

This work is licensed under a Creative Commons Attribution-Share Alike 4.0 International License
You are free to:
- Share, copy and redistribute the material in any medium or format
- Adapt, remix, transform, and build upon the material for any purpose, even commercially.
- The licensor cannot revoke these freedoms as long as you follow the license terms.




